What Should Be Included in Weekly Family Therapy Session Notes
Clear, concise, and accurate therapy progress notes are beneficial to practitioners and their clients. They're instrumental in monitoring a patient's progress, the efficacy of their treatment, and helping professionals sympathise their patient'southward personal experiences.
To be helpful and informative, though, progress notes in mental wellness need to follow some guidelines. In this overview, we'll introduce their central elements, a pace-past-step guide to writing therapy progress notes, and some of the best therapy software you can use to create excellent progress notes efficiently.
Before getting started, we recommend trying Quenza, our therapy notes software for e-mental wellness practitioners.
Quenza is a complete suite of composite care tools that includes everything you need to make and store clear, professional person therapy progress notes on a HIPAA-compliant platform.
What Are Progress Notes in Mental Wellness?
Progress notes are clinical notes fabricated by psychologists, therapists, clinical counselors, psychiatrists, and other practitioners involved in a patient'southward treatment and intendance.
More specifically, they incorporate clinical facts and medical reasoning near "the intendance delivered to patients and the clinical events relevant to diagnosis and treatment." [1]
Progress notes are professional person documents that communicate of import information on a patient's condition between multiple providers. In mental health contexts, they must be stored privately and securely in a HIPAA-compliant mode.
Divergence Between Progress & Psychotherapy Notes
Progress notes are professional person documents that communicate of import data on a patient's condition between multiple providers.
As medical and mental healthcare providers will know, progress notes play a vital part in treatment planning and service delivery across a wide range of helping professions, such as occupational, concrete, and speech therapy.
This distinguishes them from psychotherapy notes, which contain information exclusively related to a patient'due south therapy sessions. Also, unlike progress notes, psychotherapy notes are merely written by counselors, therapists, and mental health practitioners who are actively involved in their therapy.
This table outlines a few more differences between progress and psychotherapy notes.
| Progress Notes | Psychotherapy Notes | |
|---|---|---|
| Purpose |
|
|
| Written by | Any care provider involved in a patient's handling plan, e.g., Social/Instance Workers, GPs. | Psychologist, Psychiatrist, Counselor, Psychotherapist |
| Content | May include:
| May include:
|
| Privacy |
|
|
10 Steps For Writing Effective Progress Notes
Following a template is an easy way to ensure all important details and data are included in your therapy progress notes.
Many treatment software solutions offer this functionality, with a multifariousness of formats and outlines for different healthcare subsectors – psychiatry, counseling, and more.
For example, Therapy Notes comes with Psychotherapy Progress Notes templates and a step-by-step guide to help psychologists write effective progress notes. Each step corresponds with a different field in the notation, starting with patient information and ending with a digital clinician signature:[2]
- Note Header: A cursory overview of the essential practitioner, patient, and session data, such as when the appointment took place, its duration, and service codes for do administration.
- Diagnosis: ICD-10 or DMS5 codes might be relevant here if the patient has been diagnosed with a mental wellness condition.
- Patient Presentation: A clarification of how the client appears, using different modalities, e.m., cognitive functioning, bear upon, or behavior.
- Rubber Problems: Whatever important data regarding the patient's well-being.
- Medications: For prescribing clinicians such as psychiatrists and full general MDs.
- Symptom Clarification and Subjective Written report: This includes reports and direct quotes regarding the patient'south status. These may come from the client themself and/or their key caregiver and might relate to how the patient is feeling, how they view their progress, or their opinions on the mental health treatment plan.
- Relevant Content: Objective data such as test results, documents, and therapy notes might exist included here – this section is for relevant e-mental health information that could 'complete the picture' fatigued by the progress note.
- Interventions Used: This step involves documenting the treatment interventions practical and the broader field that they fall into. Examples might include cognitive restructuring within CBT or relaxation techniques as part of a mindfulness grooming program.
- Treatment Plan Progress: Each progress note should mention whether a client'south treatment plan objectives are being met.
- Signatures: Most telecounseling software includes the power to e-sign documents and store them in a secure, HIPAA-compliant style.
A Cursory Await At The Lather Method
If the step-by-step guide above seems familiar, information technology's likely because this particular therapy progress notes template leverages cardinal elements of the SOAP note format.
Soap Notes follow a standard 4-signal layout roofing critical information on a patient's health status. A specific type of progress notation, Soap notes tin be shared with any other therapists and care professionals the client may be working with.
The four sections of a Lather method note are:
- Subjective Data on a patient'southward feelings, experiences, or thoughts, such as direct quotes or their observations
- Objective Data regarding their mental or general health condition, east.g., details from their therapy appointment
- Cess Information that integrates subjective and objective details with a therapist's professional estimation, and
- Plan details regarding any adjustments or side by side steps that the counselor and customer feel are needed.
Read Writing SOAP Notes: Stride-by-Step Guide, Examples, and Templates for a lilliputian more item on what each section should feature, as well as a host of helpful formats and walkthroughs.
3 Helpful Templates and Formats
Therapy progress notes can range from the very bones to more comprehensive, detailed structures.
SOAP Notes aren't the only format used in mental health documentation. Mental wellness progress notes can range from the very basic to more than comprehensive structures, like the 10-step example Therapy Notes higher up.
To illustrate, here are some useful free templates for practitioners to utilise and download.
Quenza Therapy Notes Templates
Quenza offers free evaluation, cess, and intake certificate templates for e-counselors in its Expansion Library, including a range of forms that can exist customized to use as therapy progress note templates. The Outcome Rating Calibration, shown below, captures data on a customer's individual, interpersonal, social, and overall functioning for including in progress notes.

These insights can help practitioners continue track of how a client is progressing with therapy and can be used to populate more detailed therapy notes that include the session'due south focus, client's name, and more than. With professional therapy notes software, this is oftentimes as unproblematic as including custom fields for additional information.
SampleTemplates
SampleTemplates also provides healthcare progress notes formats for physical therapists, pediatricians, general clinicians, and therapists.
These include BIRP Note templates, Soap Note structures, integrated progress notes and billing forms, and digital samples for electronic note-taking.
HarmResearch.org
HarmResearch.org sells Psychiatric and versatile Visit Progress Notation templates for professional employ. Their psychiatric progress note template includes fields for:
- Patient demographics
- Presenting problem
- Past psychiatric history
- Diagnostic interview summaries
- Past medical history, and other key fields.
List of Interventions & Common Terminology
When documenting interventions and treatments equally part of progress note-taking, advisable language and abbreviations can greatly speed up the procedure.
Clinical terminology also ensures a common professional person language exists betwixt practitioners; information technology facilitates amend understanding and establishes a consequent frame of reference.
In therapy for mental health, appropriate terminology can be a combination of diagnostic references, such as DSM5 or ICD-x codes, and descriptive terms for subjective sections progress notes.
Mutual Terminology
The Canton of Santa Clara suggests a helpful Counselor'southward Thesaurus in its Clinician's Guide Toolkit. This covers commonly-used descriptors to particular dissimilar aspects of a client'south health, advent, and more than.[3]
The Thesaurus covers categories such as:
- Affect, Mood, or Disposition – e.1000. Lighthearted/carefree, Depressed/Down-hearted/Dispirited/Disheartened, Apartment/Shallow/Deadening/Listless
- Mental attitude – such asApathetic/Inert/Absence of Affect, Belligerent/Quarrelsome/Disagreeable
- Behavior – ideas include Over-cautious/Besides Careful, Lethargic/Sluggish, or Spontaneous/Firsthand
- Work Habits, Noesis, Orientation, and more.
Interventions
Having a listing of frequently-used interventions on hand for quick reference can be particularly useful in multi-provider contexts, helping different practitioners empathize what treatments a client is pursuing with other specialists.
In mental health disciplines, these interventions might address:[4]
- Acrimony Management for healthier self-expression
- Behavior Reinforcement, commonly part of intrinsic coaching methodologies
- Collaborative Problem-solving for human relationship counseling, family therapy, conflict resolution, and other
- Cognitive Restructuring – a idea-based CBT intervention
- Communication Skills Development – east.g., as role of interpersonal therapy
- Coping Strategies Development for addressing a diversity of mental wellness weather
- Centre Move Desensitization and Reprocessing (EMDR) for trauma counseling
- Progress/Objective Review, which might involve collaborative goal-setting as part of mental health coaching
- Identifying Triggers, as seen in therapy for substance abuse, or anger management
- Imagery – e.g., within a graded exposure handling for anxiety
- Mindfulness – covering Mindfulness-Based Stress Reduction (MBSR), Mindfulness-Based Cognitive Therapy (MBCT), and formal/breezy Mindfulness Training
- Trouble-Solving Skills Evolution – another versatile CBT intervention, and
- Stress Management – which can include both therapist-guided activities and lower-intensity Stepped Care interventions.
Individual & Group Therapy Notes: three Examples
Progress notes for private and group therapy will differ in a few ways, equally different sections may be required for distinct criteria. Their overall purpose, however, remains the same.
This ways that both documentation types should include details on the detail patient or customer'south progress overall, important identifiers, and relevant notes from the session that took identify.
The snapshot below shows part of an Individual Progress Note created using the ICANotes software, in which behavior, content of therapy, intervention, diagnoses, and treatment plan details are included:[5]

Comparison this with an ICANotes Group Therapy Progress Notation Example, we tin run across the latter varies only slightly with regard to construction and content.

Both private and group therapy notes are legal documents and must be stored securely.
Another clever style to integrate subjective information into therapy progress notes is by inviting clients to contribute their own notes from sessions.
I instance template in Quenza's Expansion Library, Session Notes for Clients , offers a structured form for patients to fill up out with insights, reflections, and other observations from a therapy appointment:
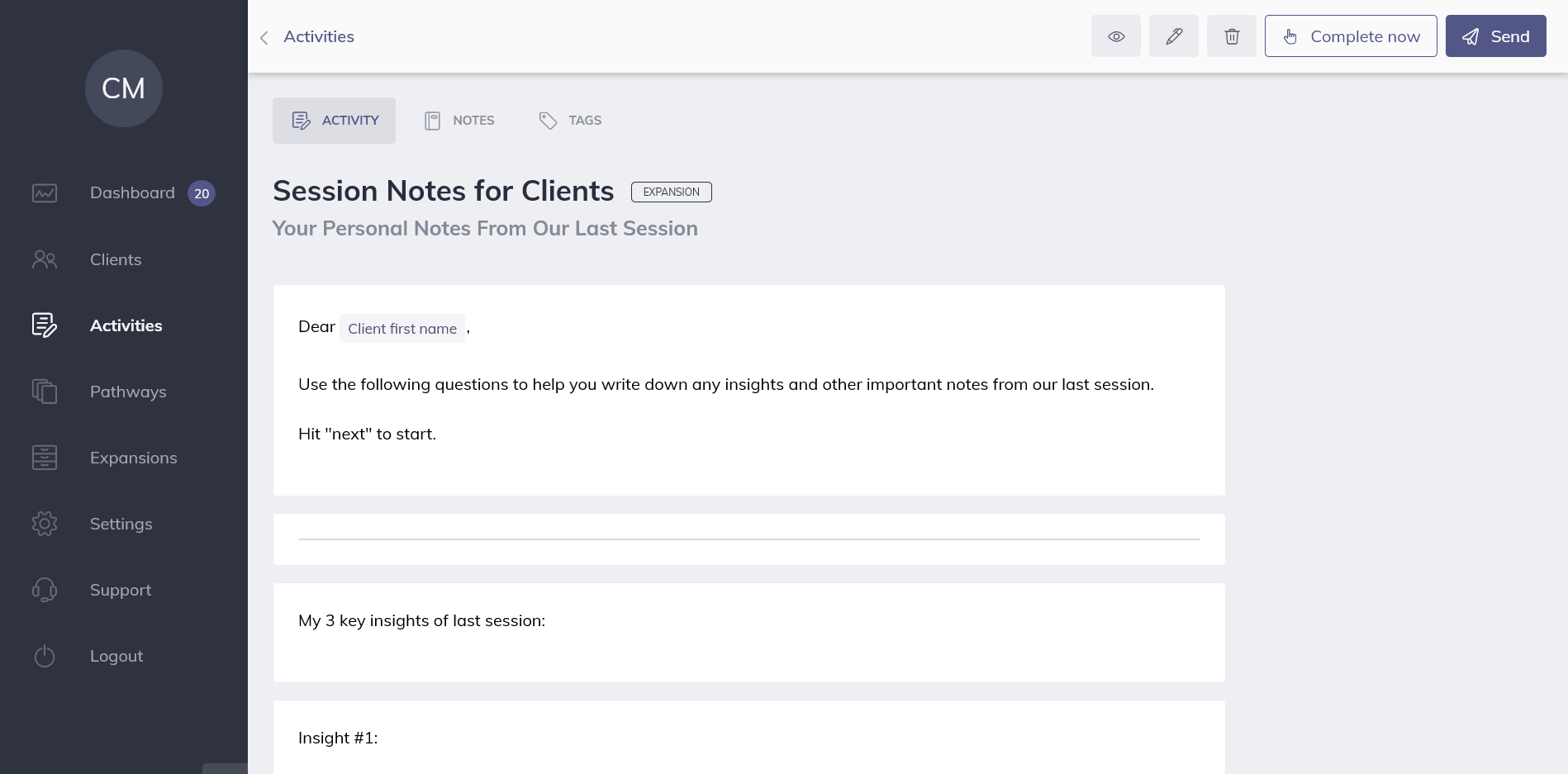
Past collecting a patient's own observations online, professionals can hands copy and paste direct quotes into their private progress notes. All data is securely stored on the i HIPAA-compliant therapy platform, and visible only to the client and their therapist.
Smart Solutions: 3 Apps and Software Systems
Whether yous're looking for a lightweight, dedicated Progress Notes software or a bigger solution, these apps and systems all come up with templates for therapists and other mental health specialists.
| Software | Details |
|---|---|
 | MyClientsPlus is a versatile mental wellness system for pocket-sized practices and solo practitioners – it's also relatively simple to utilize after an initial learning curve. With MCP'due south Therapy Progress Notes capabilities, counselors and psychologists can cull betwixt templates for psychiatry, counseling, full general psychology, and more. Within different sub-sectors, you lot'll discover even more predesigned formats to brand documentation more than effective and efficient. Examples include Therapy Intake Forms, Treatment Plans, and Client Information Forms. MyClientsPlus farther streamlines Progress Annotation creation with diagnostic codes and e-signatures and is one of the more than affordable solutions on the marketplace. |
| Name | MyClientsPlus |
| Price | $24.95+ monthly |
| Good For | Psychologists, east-Counselors, Therapists, Mental Health Coaches |
| Website | https://world wide web.myclientsplus.com/ |
| Software | Details |
|---|---|
 | Both mental health treatment plans and progress notes are piece of cake to create with Quenza's browser-based software and apps. Templates for different note types, such as Lather notes, BIRP notes, and more can be built quickly using drag-and-drop tools, and the software stores all progress notes privately and securely on a GDPR- and HIPAA-compliant organisation. Forms tin can be shared through a individual Portal on costless client iPhone and Android apps, and all progress and results are shared in real-time with the therapist. Even better, Quenza comes with a huge Expansion Library of freely customizable note templates. |
| Name | Quenza |
| Price | $1+ monthly |
| Good For | Psychologists, e-Counselors, Concrete Therapy, Voice communication Therapy, Occupational Therapy, Mental Health Coaches, Mental Health Apps |
| Website | https://quenza.com/ |
| Software | Details |
|---|---|
 | TherapyNotes has a library of Progress Note templates for solo practitioners and teams and comes with video therapy software for telehealth sessions. Psychotherapy Progress Notes, as shown above, can exist populated using clinical codes before they are linked with a client'southward appointments for easier admin and use in sessions. When a Therapy Session starts, the software automatically creates a To-Do list item reminding users to create the relevant documentation. |
| Name | TherapyNotes |
| Price | $49+ monthly |
| Good For | Psychologists, due east-Counselors, Therapists, Mental Health Coaches |
| Website | https://world wide web.therapynotes.com/ |
Final Thoughts
From basic Lather frameworks to detailed psychiatry notes, there's no one style to write a great progress notation. The way you cull to certificate your client's data is downwardly to you equally a practitioner, just hopefully, these templates, guides, and formats volition be of value.
If you're happy with your Therapy Progress Notes software, do let your fellow professionals know in a comment. If you're still on the hunt for a new solution, you'll find even more tips and advice in our comprehensive article on therapy notes software.
We hope you've found some clever ways to streamline your therapy documentation. To implement what you lot've learned, don't forget to explore Quenza'due south Therapy Progress Notes tools with your $1, thirty-24-hour interval trial.
If your goal is to take a bigger positive bear on on your clients' wellbeing, Quenza will give you everything you demand to create professional, authentic notes more than efficiently, leaving you with more than fourth dimension to focus on the mental healthcare solutions that matter.
References
- ^ Aghili, H., Mushlin, R. A., Williams, R. M., & Rose, J. Southward. (1997). Progress notes model. In Proceedings of the AMIA Almanac Fall Symposium (p. 12). American Medical Informatics Association.
- ^ Therapy Notes. (2020). How To: Complete a Progress Note. Retrieved from https://back up.therapynotes.com/article/118-how-to-complete-a-progress-note
- ^ Santa Clara County. (2008). Clinician's Guide Toolkit. Retrieved from https://www.sccgov.org/sites/bhd-p/Policies-Procedures/developed-system-of-care--policy-procedure/Documents/Clinician_Gde_toolkit.pdf
- ^ MyClientsPlus. (2020). Usually-used Intervention Words for Mental Wellness Progress Notes. Retrieved from https://myclientsplus.com/web log/unremarkably-used-intervention-words-for-mental-health-progress-notes/
- ^ ICANotes. (2020). Sample Notes Therapy Notes. Retrieved from https://www.icanotes.com/features/charting/therapy/sample-notes/
Source: https://quenza.com/blog/progress-notes/
0 Response to "What Should Be Included in Weekly Family Therapy Session Notes"
Postar um comentário